by Juan Martin Palomo DDS, MSD
by Juan Martin Palomo DDS, MSD
We all know Cone Beam Computed Tomography (CBCT) by now. It allows a non-invasive, usually less than 10-second capture of the craniofacial anatomy, which is able to create all possible traditional 2D radiographs, giving far more diagnostic information. Probably the main mentioned reason of why it has not replaced the traditional panoramic and cephalometric radiographs in clinical orthodontics, is radiation. Depending on the settings used, it could expose the patient to more radiation than that of a ceph and pano. The radiation would still be considered low, according to the American College of Radiologists, and is less than the additional annual cosmic radiation that somebody living in high altitudes, such as Colorado, receives, but nevertheless, more than a ceph and pano. But this is no longer the case, for a while.
Most major CBCT manufacturers have now a low-dose scanner in the market, which allows the 3D image to be captured, with less radiation than a panoramic radiograph. It giv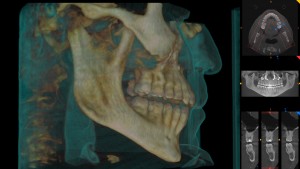 es a complete 3D image, where a pano, ceph, and complete 3D view can be used, for less radiation than that of a distorted pano. How is this possible? The answer is “capturing technology”.
es a complete 3D image, where a pano, ceph, and complete 3D view can be used, for less radiation than that of a distorted pano. How is this possible? The answer is “capturing technology”.
When a low dose 3D image is captured, the scanner does not go all 360 degrees around the patient’s head. Sometimes it is just 180 degrees. The 3D image is basically a combination of several static images (radiographs) taken while the scanner rotates around the patient’s head. In a low dose option, the number of images captured are less than 200, as opposed to the usual 300-600. When a panoramic radiograph is being taken, the x-ray beam is “on” the whole time, beeping, while going around the patient’s head. In a low dose CBCT scanning, pulse technology is used, so the x-ray beam is only “on” for a fraction of a second while taking a quick image, turning itself “on” and “off” automatically, resulting in a total radiation exposure of about 2 seconds.
All this in combination with low radiation settings, results in total effective radiation to the patient in the teens or low twenties, compared to high twenties for a pano. And in this numbers game that is effective radiation, the suggested safety threshold is 30 microsieverts. Anything below 30 microsieverts can be considered low, and fair game.
Now for the very necessary disclaimers. This does not mean that because we can get to less than 30 microsieverts we should scan everybody. Zero is still less than 30. So if a radiograph that can answer the question clinically posed has already been taken, retrieve it and do not take an additional one. If no radiograph is necessary, don’t take one just because you can. But if a radiograph is needed, and a low dose CBCT is an option, I would have a hard time justifying a ceph and pano, as opposed to a low dose CBCT. And to take a pano or ceph before taking a low dose CBCT would also be unnecessary additional radiation to the patient.
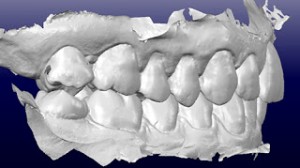
The low dose CBCT alone has more than sufficient image quality for what we need in orthodontics. I have seen images from several manufacturers, and this is clearly a situation where less radiation to the patient is also more information to the doctor. What better win-win that this can we ask?